Unlocking Joint Youth: How Inhibiting 15-PGDH Could Redefine Osteoarthritis Treatment
Osteoarthritis (OA) silently erodes joint cartilage, turning daily movement into pain for millions. Current options—painkillers, therapy, or knee/hip replacement—manage symptoms but fail to restore lost tissue. A 2025 breakthrough from Stanford changes this narrative by targeting 15-hydroxyprostaglandin dehydrogenase (15-PGDH), an enzyme dubbed a “gerozyme” for rising sharply with age and suppressing repair.
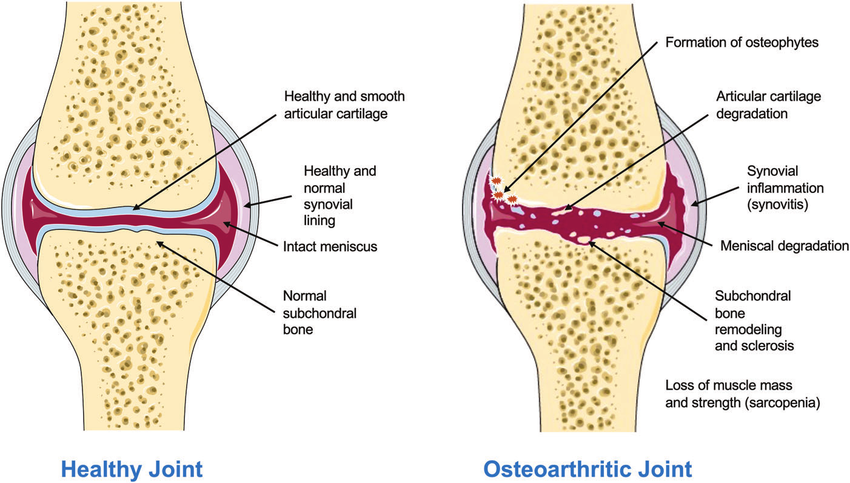
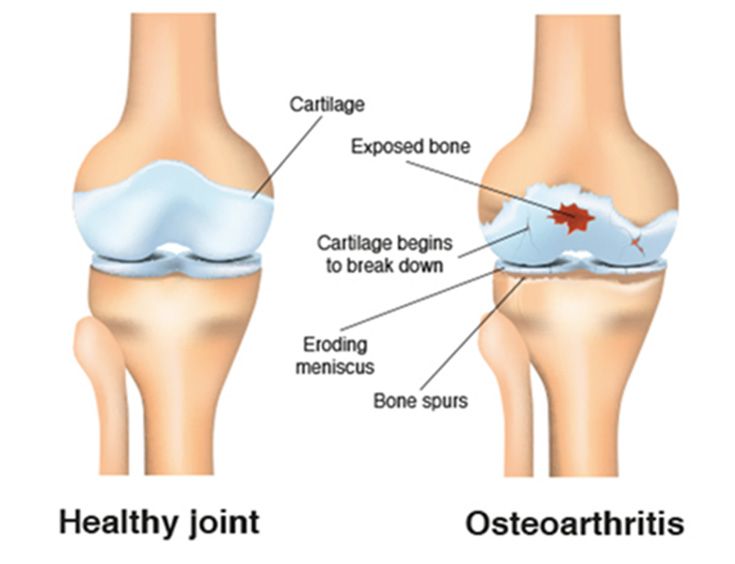
In healthy joints, smooth hyaline cartilage cushions bones. In OA, it thins, roughens, and inflames, narrowing space and causing stiffness.
The study (Science, November 2025) revealed 15-PGDH doubles in aged/injured mouse cartilage, degrading prostaglandin E2 (PGE2)—a molecule vital for reducing inflammation and supporting chondrocyte (cartilage cell) health. High 15-PGDH shifts chondrocytes toward a hypertrophic, breakdown-prone state, accelerating degeneration.
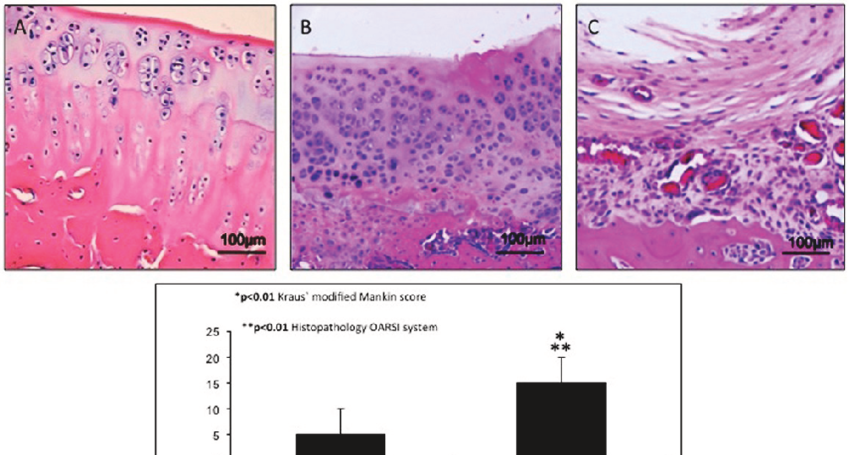
Using a small-molecule inhibitor (PGDHi, similar to SW033291), researchers blocked the enzyme. Systemic or local joint injections in old mice thickened worn cartilage surfaces. In injury models mimicking human ACL tears, post-treatment prevented OA development—mice stayed mobile with near-normal gait and reduced pain sensitivity.
Remarkably, regeneration stemmed from existing chondrocytes reprogramming via gene expression shifts, not stem cell recruitment. Treated cells produced more extracellular matrix while cutting fibrocartilage and degradation markers.
Human validation came from ex vivo tests on knee replacement tissue. One-week inhibitor exposure lowered 15-PGDH, suppressed breakdown genes, and initiated articular cartilage regrowth—hinting at clinical relevance.
This differs from past approaches relying on stem cells or growth factors, which face delivery and safety hurdles. 15-PGDH inhibition leverages the body’s own repair machinery by preserving PGE2, offering a simpler, potentially oral or injectable path.
An oral 15-PGDH blocker is already in early human trials for sarcopenia (age-related muscle loss), showing safety. OA-specific trials could follow soon, potentially transforming care by 2030.
Challenges remain: long-term safety, optimal dosing (systemic vs. intra-articular), and efficacy in advanced human OA where cartilage is minimal. Yet the mechanism—countering a core aging driver—positions it as a true disease-modifying therapy.
This work bridges geroscience and orthopedics, suggesting 15-PGDH inhibition could extend to other age-related tissues. For OA patients facing surgery, it represents hope: not just living with joint pain, but reclaiming youthful cartilage and mobility.

